Baker signed into law on New Year’s Day a multi-faceted health care bill that requires insurance companies to cover telehealth visits the same way they cover in-person care, and provides a short-term model for how those services will be paid.
The COVID-19 pandemic has strained the health care system in myriad ways over the past year, but Gov. Charlie Baker said Friday that a "silver lining" of the public health crisis is that reforms like telehealth were able to be tested, and proved effective.
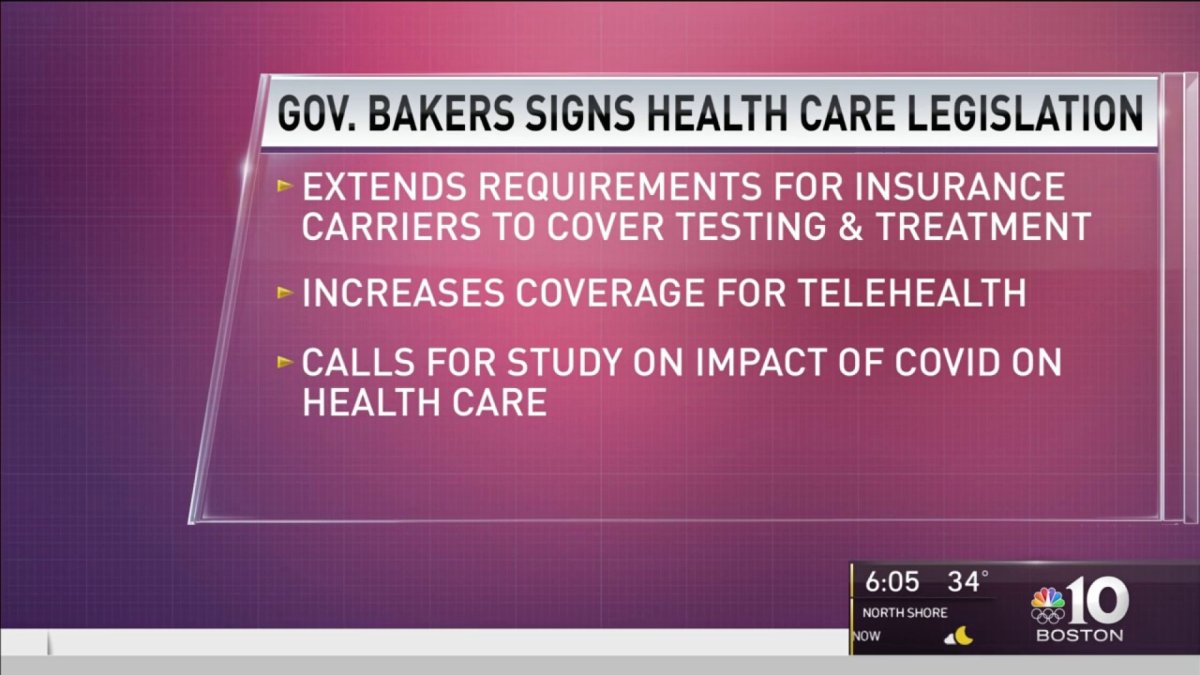
Baker signed into law on New Year's Day a multi-faceted health care bill that requires insurance companies to cover telehealth visits the same way they cover in-person care, and provides a short-term model for how those services will be paid.
The new law also protects coverage for COVID-19 testing and treatment, expands the scope of practice for advanced practice nurses and optometrists, addresses surprise out-of-network billing by requiring patient notification before non-emergency procedures and gives community hospitals two years of enhanced Medicaid reimbursements.
The final bill was negotiated by new House Speaker Ron Mariano and Sen. Cindy Friedman, but Baker said "thematically" it addressed a lot of the issues he tried to tackle in health care bill filed over a year ago.
"In the midst of all the other difficult and tragic and terrible news around health care in 2020, this is actually a really positive story for patients and practitioners," Baker said.
In an interview with the News Service, Baker said he thought the pandemic, in some ways, helped generate the momentum needed to convince policymakers to make some of the changes embraced in the new law.
Local
In-depth news coverage of the Greater Boston Area.
And as the pandemic continues, Baker said he believes the new law will be effective in giving patients better access to primary and behavioral health care that will both improve health outcomes and control costs by keeping people out of costlier emergency and inpatient care settings.
"This is a little bit of a silver lining, the experience people had with some of these issues in 2020 and as a result the Legislature baked it into state law," Baker said. "The concern that people always had with some of this stuff was whether it would be effective. Will it be useful? I think the practical experience helped get some people there."
Baker filed a comprehensive health care bill in October 2019 before the pandemic changed people's priorities and focus on Beacon Hill and put the health care system under a microscope. That bill proposed to do many of things the law he signed Friday will accomplish, including equal insurance coverage for in-person and telehealth services.
The main thrust of Baker's 2019 bill, however, was to require providers and insurers to boost their spending on addiction services, behavioral health, primary care and geriatric services by 30 percent over three years.
The compromise legislation he signed Friday does not provide the same type of financial incentive to refocus the health system on preventative care, and Baker said it may be something he returns to.
"Our health care community is spectacularly competent and tired, and I certainly think we will come back to some of these issues that were probably too big and too complicated to deal with in the context of what the last year was like, but not until after the pandemic," he said.
The bill also does not address the high-cost of some prescription drugs, which Baker and the Senate both tried to tackle this session before the pandemic.
Baker said the authority given in 2019 to MassHealth to directly negotiate with pharmaceutical companies should give lawmakers valuable information in 2021 if they return to the issue of prescription drug costs.
The new law requires insurers to permanently reimburse for behavioral telehealth at the same rate as in-person treatment, and mandates rate parity for two years for primary and chronic disease care.
Baker said he thinks the two-year window will be sufficient to figure out how to pay for telehealth services long-term and determine how the expansion of telemedicine impacts the overall cost of care throughout the system
"I've thought for a long time that because as a country we underinvest in primary care and behavioral health services a lot of people who could be treated in the community end up in the hospital and we will basically have a chance here to study this question," Baker said.
"I think we'll discover that by investing more or giving people more options to access care and supports they will stay healthier and spend less time in the hospital," he said.
After talks last session to stabilize community hospital finances collapsed, the compromise bill the Legislature put together in the closing days of this two-year session also provides a short-term boost for cash-strapped hospitals that serve low-income patient populations.
Community hospitals that serve a high percentage of low-income patients will be eligible for enhanced monthly Medicaid payments, with eligible hospitals receiving a 5 percent bump in their average monthly Medicaid payment at a collective cost of up to $35 million a year.
The health system reforms signed into law Friday come on top of measures that were included in the fiscal year 2021 budget and supported by the administration, including the use of standard provider credentialing forms by insurers and a prohibition on additional costs for same-day billing for multiple primary care and behavioral health visits.
The law also touches on some areas of the health care system than Baker did not address in either his bill or the many executive orders he has issued since the start of the pandemic. including the addition of a nurse with expertise in "innovative treatments for patient care" to the Health Policy Commission board.
"That wasn't in our bill, but it's a good thing," Baker said.
The new law also allows for reimbursements of reasonable travel and accommodation expenses for a cancer patient to participate in a clinical trial.